Medication for Infant Reflux? Why You Should Probably Pass
April 9, 2018
One of the most common concerns from parents of newborns revolve around the issue of reflux. “My baby has been spitting up – do you think she has reflux?” or “My baby has been fussy this week – do you think it’s because of reflux?” These are questions I hear all the time, both in the office and online, often paired with, “Does my baby need medication to stop acid reflux?”
Parents are quick to be concerned about reflux, because spitting up is a regular part of most babies’ everyday lives. The key is to know the difference between typical spit up and pathological reflux (which is known in the medical community as GERD – Gastroesophageal Reflux Disease).
Reflux Symptoms In Babies — What’s Normal and What’s Not
To better understand why babies spit up, and how GERD happens, we must first take a look at newborn gastrointestinal anatomy.
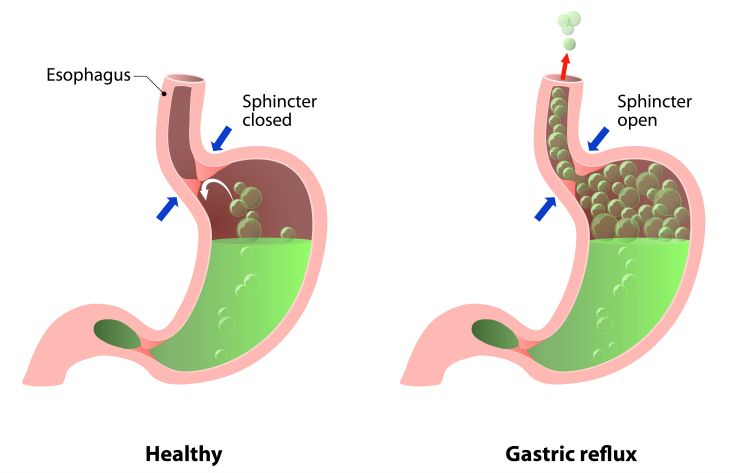
When newborns swallow breastmilk or formula, it goes through their mouth and down their esophagus. Between the end of the esophagus and the stomach, we have a ring of muscle called the lower esophageal sphincter (LES). It’s very important for all new parents to know what the LES is and how it works.
In older children and adults, this sphincter is usually quite strong and helps to keep the content of the stomach in the stomach. In newborns, this muscle is NOT mature. It is hypotonic, which means it has low tone and strength. Because this muscle is not strong enough yet to close off the food contents in the stomach, it is VERY easy for breastmilk or formula to slosh right back up the esophagus. When this happens, the process is referred to as uncomplicated gastroesophageal reflux. This process of reflux happens in ALL newborns and babies. (As adults age, this sphincter often becomes weaker and hypotonic again, which is why you may have heard your dad or grandpa talking about his GERD issues.)
If the stomach contents make it all the way back up the esophagus and through the mouth or nose, we would call this spit up. Spit up is a form of reflux, and it is extremely common. In fact, approximately 50 percent of infants between birth and 3 months have at least one episode of spitting up per day. Half. That’s a lot of babies (and even more loads of laundry)!
I see parents frequently use the term silent reflux online. It sounds scary, but what does it mean? The medical community doesn’t use this term at all, because, biologically speaking, “silent reflux” is no different than gastroesophageal reflux. Silent reflux is simply not seen, meaning that the stomach contents slosh back up into the esophagus, but it doesn’t result in spit up (coming out the mouth or nose). The infant will generally re-swallow the fluid in the esophagus to push it back down to the stomach. As I mentioned above, ALL babies will have so-called “silent reflux” at one point or another, because all babies experience gastroesophageal reflux (whether you see spit up or not). This isn’t scary, it’s biologically normal.
We must also remember that newborns and young infants lie flat most of the time, and they are on a liquid diet. The cards are stacked against all newborns when it comes to reflux. In addition to a weak LES, these factors definitely contribute to the natural and normal mechanics of reflux. Furthermore, infants who are born prematurely may have a lower esophageal sphincter that is further underdeveloped than their full-term counterparts.
Here is the bottom line: All newborns will experience Gastroesophageal Reflux, but very few babies have Gastroesophageal Reflux Disease (GERD).
Gastroesophageal Reflux becomes Gastroesophageal Reflux Disease (GERD) when acid in the stomach reflux causes irritation or injury to the esophagus, failure to grow, or additional issues like aspiration (inhalation of stomach contents to the lungs). A global, evidence based consensus defined GERD this way, “GERD is present when the reflux of gastric contents causes troublesome symptoms and/or complications.”
I know this definition can seem gray to many parents. What’s troublesome to one baby, isn’t troublesome to another. However, true GERD is when the acidity of the stomach contents is causing biological irritation, damage, and/or pain to the esophagus.

Gastroesophageal Reflux and Gastroesophageal Reflux Disease Have Different Symptoms
Normal Symptoms of Gastroesophageal Reflux:
- Spitting up (even regularly!)*
- Hiccupping
- Swallowing or gulping reflux back down to the stomach occasionally
- Normal weight gain
*Important: some irritability with spit up is totally normal (especially if spit up goes through the nose). On the other end of the spectrum, some babies will spit up and even smile at you! It’s quite common. We call these babies “happy spitters.” That is a great sign that they have uncomplicated gastroesophageal reflux that will simply resolve as they get older. If the spit up doesn’t bother your baby, don’t let it bother you!
Symptoms of Gastroesophageal Reflux Disease:
- Poor weight gain (or failure to thrive)
- Difficulty or painful swallowing during feeding
- Refusing to eat
- Choking while spitting up
- Arching of the neck or back
- Forceful or projectile vomiting
- Spitting up blood
- Recurrent cough or wheeze
- Extreme, recurrent irritation while spitting up (crying or screaming that is very difficult to soothe and happens consistently after almost every feeding)
I want to stress that most of these symptoms should be observed in a reoccurring pattern to help determine if a baby has GERD. If a baby is just irritable from a feeding every now and again, it is extremely unlikely the stomach contents are damaging their esophagus and therefore it wouldn’t qualify as GERD.
Why do we not want to jump to immediately using medications for reflux?
There are two major types of acid-suppressing medications used for infants with GERD: histamine-2 receptor antagonists (most commonly Zantac) or proton pump inhibitors (most commonly Prevacid).
Approximately 8% of infants have received a prescription for acid-suppressive therapy. The FDA found an 11-fold increase in new PPI prescriptions between 2002-2009. That is a very high amount, and I can tell you from clinical experience that many of these babies simply don’t need it. These medications are being over-prescribed, because most parents don’t understand or accept that reflux is normal and babies will outgrow it with time.
What Parents Need To Know About Reflux Medication For Babies
There are several things parents should know before giving these acid-suppressing medications a try. Let me list a few.
1. Using acid-suppressing medication does NOT typically reduce the volume of spit up.
This is the biggest myth about using reflux medications that I encounter from parents. Even after starting the medication, you will probably see the same about of spit up. You can’t beat time when it comes to the anatomy of reflux. Zantac isn’t going to make the lower esophageal sphincter get stronger faster.
Acid-suppressing medications are simply going to try to suppress some of the stomach acidity, so when the stomach contents do naturally reflux into the esophagus because of the weak LES, it is less painful or annoying.
2. It may reduce stomach acidity, but whether that helps with irritability is sometimes a toss-up.
I always like to remind moms that there are MANY different things that affect newborn irritability. Irritability is not always from reflux. Colic, being overly tired, feeding difficulties, the way the wind blows… you name it. Some newborns are just fussier than others. I know how hard and stressful that can be on moms.
Work with your pediatric provider to try and determine a cause for your baby’s irritability or fussiness. But know that sometimes when you’ve ruled out medical causes for irritability, fussiness is just a part of the newborn phase. Infants typically cry a total of one to three hours a day. I promise, fussy newborns get happier with time. This season won’t last forever.
For the babies that do have GERD and try acid-suppressing medications, I can tell you from clinical experience, sometimes it makes certain babies less irritable and sometimes it doesn’t. Don’t get me wrong, there are times when these medications drastically help with GERD symptoms, but parents should know that it’s not a sure bet. Several clinical trials have shown that reflux medications do not work better than placebos for infants with reflux disease.
For all of these reason, if you do decide to try an acid-suppressing medication, try it for a short time. These medications are relatively fast-acting. If you haven’t seen any changes or improvements within 2 weeks of use, follow up with your pediatric health provider. There is no reason to keep babies on medications that aren’t making a difference.
Also, changing the acidity of the stomach doesn’t come without some risks…
3. The clinical benefit of using acid-suppressing medications ALWAYS needs to outweigh the risk of side effects.
Most recently, a study of 800,000 children published by JAMA Pediatrics found that infants treated with acid-suppressing medications, either histamine-2 receptor antagonists or proton pump inhibitors, had a significantly higher risk of later developing allergies, especially food allergies.
As the main researcher of the study said:
“These medications are usually given to infants who regurgitate food and appear fussy. For most infants, though, regurgitation of food is not a disease. Rather, it’s a developmentally normal process.”
The research is growing that the microbe (bacteria) of the infant gut is closely linked to the development of a healthy immune system. We are learning that the more we intervene with medications that change that gut microbiome, the more likely children are to develop allergies.

There Are Natural Remedies For Reflux
There is good news for all our babies experiencing uncomplicated gastroesophageal reflux or gastroesophageal reflux disease – some natural remedies really can help! Always try these things at home before trying acid-suppressing medications.
Positioning therapy
Try to hold your baby upright for 20-30 minutes after each feeding. Babies that are laid down right after eating have difficulty keeping their food in their stomach (especially because of that weak LES). If you are holding them upright for 20-30 minutes after eating, it allows them to have more time for the food to pass through their stomach and into the intestines. This can greatly help with reflux.
Some night time feedings can be very hard for parents to stay awake for an additional 20-30 minutes to keep their baby upright. I understand. It is extremely dangerous for parents to fall asleep holding infants, especially on couches or recliner chairs, due to the high risk of SIDS. Even if your child has reflux, it is better for them to fall asleep in their own bed on a firm, flat mattress.
Before we knew that placing a baby on their stomach to sleep drastically increased the risk of SIDS, some providers would recommend that as method to help with reflux. However, the guidelines are clear:
“The risk of death from sudden infant death syndrome outweighs that from gastroesophageal reflux, in infants from birth to 12 months with GERD, supine position (laying a baby on their back) is recommended.”
SIDS still tragically kills thousands of babies every year, so the risk of death from SIDS in almost every case is drastically greater than the threat of GERD.
Offer smaller amounts of food more regularly
Overfeeding can contribute to reflux. We all know that some babies get REALLY excited to eat. While adorable, if babies eat too much, it can increase reflux and result in more spit up. If this is happening persistently with your baby, offer smaller amounts during their feedings, but make their feedings more regular.
Breastfeed if you can
Formula-fed infants do have increased esophageal acid exposure compared with breast milk-fed infants. While we completely understand that not all moms are able to breastfeed, breastfeeding or pumping is a great way to reduce acid during feedings if you can!
Monitor breastfeeding mom’s diet or use sensitive formulas
We know that certain foods that moms eat can cause more irritation than others among breastfed infants. Many of the moms I work with have seen improvement in their infant’s reflux symptoms by cutting out coffee and spicy food from their diets.
Studies report that 15 to 40 percent of infants with reflux have a cow’s milk protein intolerance. This intolerance usually improves naturally by around 12 months, but in the mean time, breastfeeding moms can try eliminating milk products from their diet. Moms may need to eliminate soy products, as well. Talk to your healthcare provider before deciding if further foods should be eliminated (mom’s nutrition is very important, too!). When eliminating foods, it usually takes at least 2-3 weeks to see if the dietary change will help your infant.
Parents of formula-fed infants can discuss the possibility of starting a hypoallergenic formula without cow or soy proteins with their provider, but again, this only helps reflux among infants that have a strong intolerance to those proteins.
Thickening feedings
Sometimes thickening feedings with infant cereal may help with reflux. However, because adding cereal increases caloric density, it can lead to increased weight gain. The recommendation for starting infants on cereal or solid food is 4-6 months. If you are concerned about reflux, and want to try thickened feedings sooner than that, talk to your provider about it first.
So, where does this leave parents who have a baby with reflux?
Gastroesophageal reflux isn’t a simple issue, but remember, this is a normal phase of infancy. It gets better with time! Spitting up occurs in 50% of infants from 0 to 3 months, 67% in 4-month olds, and 5% in 10–12 month old infants. Take encouragement that reflux almost always resolves spontaneously, in nearly all of these infants, without medication.
If you are concerned about your baby’s reflux, and seeing symptoms of GERD, keep a log of when your baby experiences troubling symptoms or complications. That will help your child’s healthcare provider in their diagnosis when you bring them in for a checkup.
Author: Dani Stringer, MSN, CPNP, PMHS – founder of KidNurse and MomNurse Academy